From Misinformation to Implementation: Why Modern Medicine Needs a Guideline-to-App Industrial Complex
By Chukwuma I. Onyeije, MD, FACOG
Maternal-Fetal Medicine Specialist, Medical Director at Atlanta Perinatal Associates, Founder of CodeCraftMD

I was reviewing evidence-based counseling guidelines for low-dose aspirin in preventing preeclampsia when something bothered me.
Not the science—that was solid. The Society for Maternal-Fetal Medicine recommendations are clear, the evidence is strong, and the logic holds up under scrutiny.
What bothered me was the final delivery mechanism: a static PDF handout.
Meanwhile, on TikTok, a wellness influencer with zero medical training was explaining why aspirin is “toxic” and “Big Pharma’s way of poisoning pregnant women.” The video had 2.3 million views, thousands of shares, and was algorithmically optimized to find exactly the patients I counsel every week.
That’s when I realized something: medicine isn’t losing the misinformation war because we lack evidence. We’re losing because we’re bringing paper to a software fight.
The Misinformation Industrial Complex Has Already Won the Infrastructure War
Health misinformation today isn’t random. It’s industrialized:
- Dynamic: Content evolves based on engagement metrics and trending concerns
- Algorithmically amplified: Platforms optimize for emotional response, not accuracy
- Visually compelling: Short videos, infographics, interactive stories
- Always accessible: Lives on phones, revisited multiple times, shared effortlessly
- Continuously iterated: Creators A/B test messaging, adjust language, respond to comments in real-time
Evidence-based medicine, by contrast, relies on:
- One-time counseling sessions
- Dense paragraphs of text
- Static documents that cannot update once printed
- Materials designed for reading, not interaction
- Distribution that ends when the patient leaves the office
This isn’t a fair fight. We’re countering a living, adaptive system with fossils.
What I Built in an Hour (And What It Taught Me)
As a physician-developer, I did what we do: I built something.
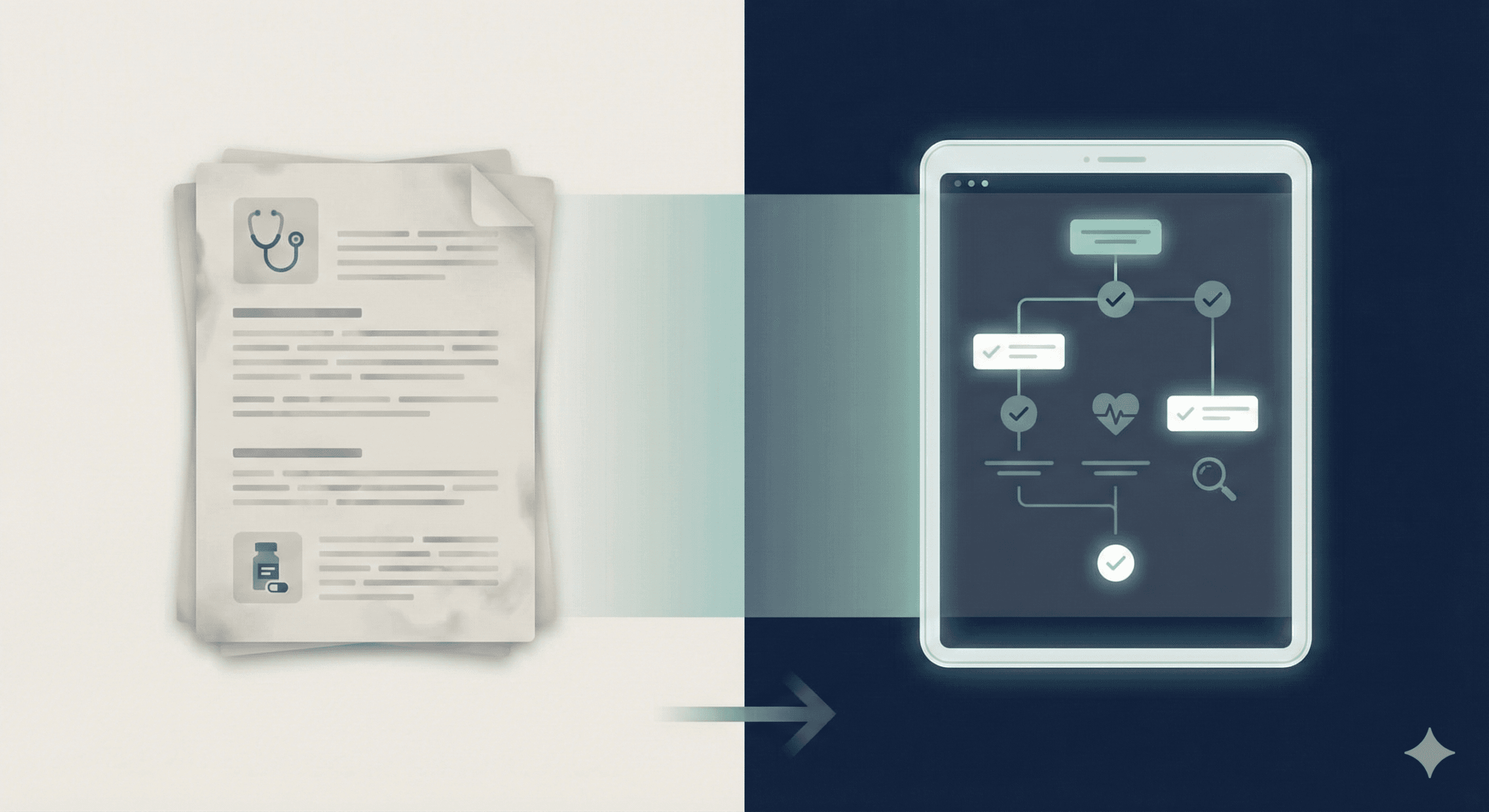
I took the aspirin counseling framework—the same evidence, the same clinical logic—and translated it into an interactive web app. Not a complex application. Just a decision tree that walks patients through:
- Why they might qualify for low-dose aspirin
- What the evidence shows about preeclampsia prevention
- What the actual risks and benefits are
- What happens if they choose not to take it
Same information. Completely different interface.
And that’s when the bigger realization hit me: most clinical guidelines are already software—we just haven’t compiled them yet.
Every Guideline Is Already an App We Haven’t Built
Think about modern clinical guidelines. What do they actually contain?
- Decision trees and flowcharts
- Inclusion and exclusion criteria
- Risk stratification algorithms
- Step-by-step counseling logic
- Conditional recommendations based on patient factors
This is computational logic. It’s software disguised as prose.
The problem is that we’ve been rendering software as static documents. We take something inherently interactive—a decision tree—and flatten it into paragraphs that patients skim, misunderstand, or never revisit.
Every major clinical guideline from ACOG, SMFM, AHA, ACC, USPSTF, or any other professional society is already an app. We just haven’t built it yet.
Why Interactive Clinical Apps Outperform Static Handouts
This isn’t about novelty. It’s about structure. Here’s what physician-built interactive tools do that static handouts cannot:
1. Real-Time Adaptability
Guidelines change. New evidence emerges. Criteria shift. Language evolves to address patient concerns.
When ACOG updates a recommendation, a web app can reflect that change instantly—globally, for every patient who uses it. A printed handout cannot. Even digital PDFs require redistribution.
In my practice at Atlanta Perinatal Associates, I’ve watched guidelines for fetal aneuploidy screening evolve significantly over the past decade. Every update meant reprinting hundreds of handouts, hoping nurses grabbed the current version, and knowing some patients were still reading outdated materials.
An app updates once. Everywhere. Immediately.
2. Persistent Access and Reinforcement
Patients lose papers. They don’t lose their phones.
An interactive tool becomes a reference patients can return to—before their appointment to prepare questions, during the visit to follow along, and after the visit when new concerns arise.
This isn’t replacing counseling. It’s extending clinical reasoning into the spaces where patients already live: group chats, late-night Google searches, conversations with family members.
3. Active Engagement vs. Passive Reading
Reading is passive. Interaction is active.
When a patient clicks through decision logic—”Why do I qualify? What does this prevent? What are the actual numbers?”—they’re not just consuming information. They’re participating in clinical reasoning.
This cognitive engagement deepens understanding in ways that reading paragraphs never does.
4. Preserved Nuance Without Oversimplification
This is the counterintuitive part: apps can preserve clinical nuance better than dense text.
Decision logic can unfold step by step. Conditional information appears only when relevant. Uncertainty can be honestly presented without overwhelming the patient.
Handouts force us to choose between completeness (dense, unreadable) and simplicity (loss of nuance). Interactive tools escape that false choice.
The Clinical Developer’s Unique Position
Anyone can code. Anyone can create health content.
But only physician-developers can:
- Preserve the clinical nuance that matters
- Respect uncertainty instead of manufacturing false confidence
- Know when not to build something because clinical judgment can’t be algorithmatized
- Anchor tools in professional standards and evidence hierarchies
- Understand the liability landscape and practice within it
This is why vendor-built health apps so often miss the mark. They’re built by engineers who don’t understand medicine or by clinicians who don’t control the codebase.
When physicians build—or directly shape—these tools, software stops being a liability and becomes clinical infrastructure.
This is the core ethos behind Doctors Who Code.
Building Counter-Infrastructure to Misinformation
If misinformation thrives because it’s dynamic, adaptive, and omnipresent, then evidence must meet it on those same structural terms.
Interactive, physician-built clinical apps are not gimmicks. They’re counter-infrastructure:
- They reinforce evidence outside the exam room
- They compete for attention ethically, using the same engagement mechanics that make TikTok effective—but anchored in evidence
- They scale truth without sacrificing rigor
- They occupy the same contested digital spaces where patients make decisions
Every viral misinformation video represents a failure of delivery, not a failure of evidence. We have the truth. We just haven’t built the right interfaces for it.
The Guideline-to-App Vision
Imagine if:
- Every ACOG practice bulletin shipped with an interactive patient-facing version
- SMFM clinical guidance included decision tools patients could use at home
- AHA/ACC risk calculators were embedded in apps patients already trust
- Updates propagated instantly instead of waiting years for reprints
- Counseling became something patients interacted with repeatedly, not something handed to them once
This isn’t futuristic. This is achievable now.
The technology exists. The evidence exists. The guidelines exist.
What’s missing is the infrastructure to compile evidence into interfaces that patients will actually use.
A Call to Action for Physician-Developers
The future of medicine will not be decided by who publishes the best evidence.
It will be decided by who builds the best interfaces for truth.
If you’re a physician who codes—or who’s learning to code—this is your moment. The clinical guidelines you reference every day are already computational. They’re waiting to be built.
If you’re a physician who doesn’t code but understands this problem, you can:
- Collaborate with engineers who respect your clinical judgment
- Identify which guidelines in your specialty desperately need interactive versions
- Advocate within your professional societies for digital-first guideline development
The misinformation industrial complex has had a decade-long head start. But they don’t have what we have: evidence, rigor, and the clinical judgment to know when software helps and when it doesn’t.
Final Thought
Every guideline is already an app.
The only question is whether we’re willing to compile it.
About the Author
Chukwuma I. Onyeije, MD, FACOG, is a board-certified Maternal-Fetal Medicine specialist and Medical Director at Atlanta Perinatal Associates, where he specializes in managing high-risk pregnancies. He is the founder of CodeCraftMD, an AI-powered platform for medical billing and clinical documentation, and runs the Doctors Who Code blog, which explores the intersection of clinical medicine and software development. Dr. Onyeije advocates for physician-built healthcare technology as essential clinical infrastructure and regularly writes about how physicians can leverage coding skills to improve patient care and counter medical misinformation.
Dr. Chukwuma Onyeije emphasizes the critical role of physician-designed applications in enhancing clinical decision support and ensuring adherence to evidence-based medicine. He argues that by integrating digital health tools into their practice, physicians can provide interactive patient education that effectively counters the pervasive spread of medical misinformation. This approach not only fortifies the quality of patient care but also aligns with the guidelines set forth by organizations such as ACOG and SMFM, particularly in the realm of maternal-fetal medicine. Ultimately, the collaboration between healthcare professionals and technology developers is paramount in establishing a resilient healthcare infrastructure.
Related Reading:
- Why Physicians Should Code: Beyond EMR Frustration
- Building Clinical AI Tools: A Physician-Developer’s Framework
- The Contested Clinical Space: Why Social Media Is a Medical Issue
Tags: physician-developer, medical misinformation, clinical decision support, healthcare technology, evidence-based medicine, interactive patient education, digital health tools, clinical guidelines, ACOG, SMFM, maternal-fetal medicine
SEO Title: Why Medicine Needs Physician-Built Apps to Fight Misinformation | Doctors Who Code
Meta Description: Maternal-Fetal Medicine specialist Dr. Chukwuma Onyeije explains why interactive, physician-built clinical apps are essential counter-infrastructure to combat the industrialized spread of health misinformation.