How I Used Code (and AI) to Fix One of Healthcare’s Most Painful Bottlenecks: Prior Authorizations
In the world of high-risk pregnancy, minutes matter. Whether we are managing a case of preeclampsia or coordinating a fetal intervention, the clinical stakes are immense. Yet, as a Maternal-Fetal Medicine (MFM) specialist, I’ve found that the biggest hurdle to patient care often isn’t the pathology—it’s the paperwork.

Specifically, the Prior Authorization (PA).
At CodeCraftMD, we believe that when physicians understand the “logic” of software, we stop being victims of inefficient systems and start becoming the architects of their solutions. Here is how I applied a “Doctors Who Code” mindset to solve one of medicine’s most notorious administrative bottlenecks.
I. The Invisible Friction in Healthcare
To a patient, a doctor’s order feels like the final word. In reality, it’s often just the start of a negotiation. A Prior Authorization is essentially a request asking an insurer, “Is this medically necessary, and will you pay for it?”
While designed to control costs, PAs have evolved into a massive engine of friction. They impact:
- Specialized Medications: Life-saving biologics or anticoagulants.
- Advanced Imaging: Detailed fetal echos and targeted ultrasounds.
- Medical Devices: Continuous glucose monitors or insulin pumps.
The Insight: Prior authorizations aren’t just an administrative chore; they are a data-translation problem that introduces dangerous delays for patients and burnout for clinicians.
II. The MFM Struggle: High Stakes, High Paperwork
At My MFM practice, my patients require frequent surveillance. Every ultrasound, every consult, and every specialized lab can trigger a new PA.
The process was always the same: a medical assistant or nurse would have to comb through pages of ultrasound reports and clinical prose to find specific diagnosis codes (ICD-10) and procedure codes (CPT). They then had to synthesize this into a “clinical justification” written in the specific “payer-speak” the insurance company requires.
The data already existed in the Electronic Health Record (EHR), but it was trapped in unstructured notes. We were losing hours to manual “copy-and-paste” cognition.
III. The “Aha” Moment: This Is a Coding Problem
As I worked on my various health-tech builds, it hit me: the PA form is just a structured representation of the data already in the patient chart.
If the data is there, and the form is the target, the gap between them is simply a transformation layer. I asked myself: What if software could extract exactly what insurers want—without making things up?
IV. Designing a Safer AI Workflow (No Hallucinations Allowed)
When applying AI to clinical workflows, the margin for error is zero. We cannot tolerate “hallucinations”—fabricated lab values or invented diagnoses. To bridge this gap I focused on three pillars:
- HIPAA Compliance: Ensuring all data handling meets federal privacy standards.
- Source-Grounded Outputs: The AI is instructed to only use provided text. If it isn’t in the note, the AI cannot “infer” it.
- Explicit “Missing Data” Flags: If the insurer requires a BMI and it’s not in the report, the system must flag it rather than guess.
V. The Technical Build: From Prose to Form
The workflow I developed involves a specialized “Clinical Extraction Engine.” Here is the logic:
- Inputs: We feed the system the patient’s clinical ultrasound report and the specific insurance requirements.
- The Processing Layer: Using a structured prompt within a HIPAA-compliant LLM, we extract:
- Validated ICD-10 & CPT Codes: Directly supported by clinical evidence.
- High-Risk Indicators: Identifying specific maternal or fetal comorbidities.
- Automated Justification: Generating a draft letter that mirrors the payer’s medical necessity criteria.
- The Gap Analysis: The system identifies missing fields (e.g., “Missing: Last LMP date”) so the staff knows exactly what to look for.
VI. The Human-in-the-Loop Model
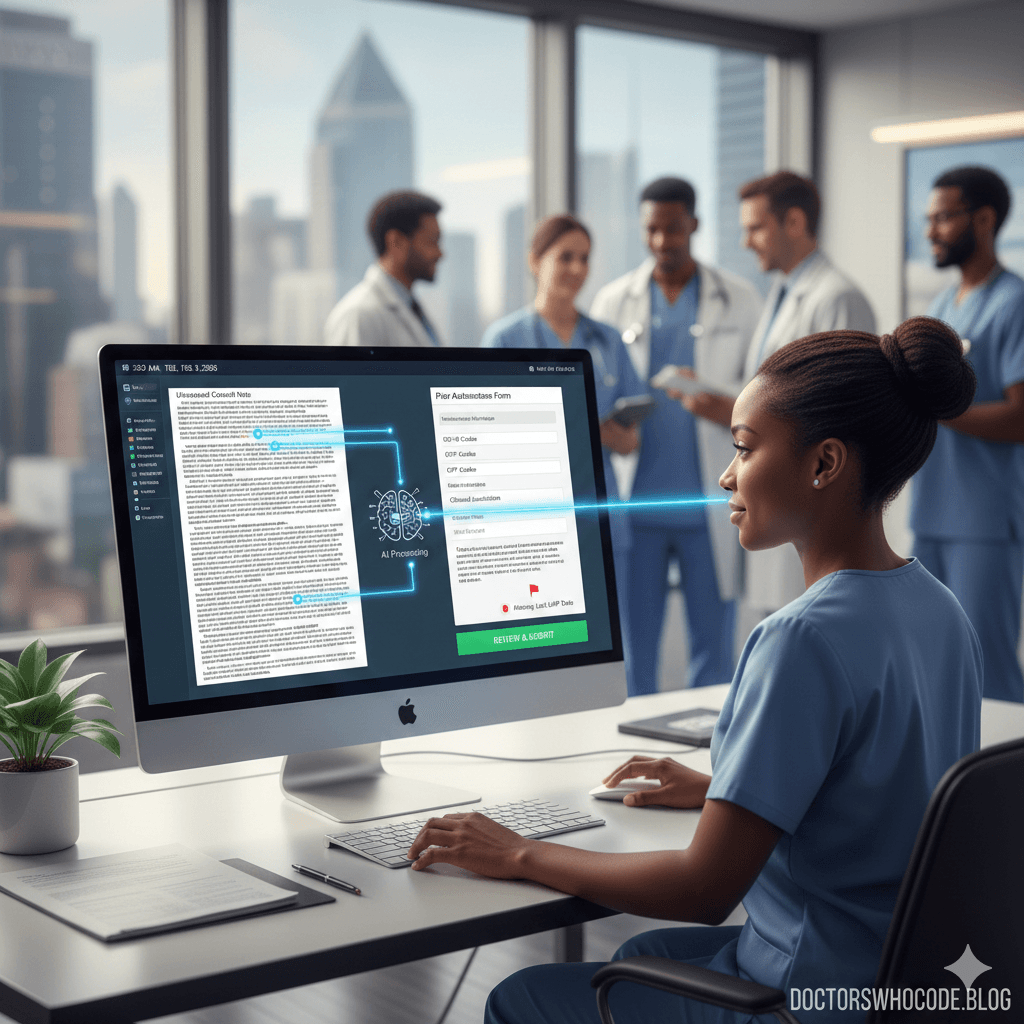
We advocate for Augmented Intelligence, not replaced intelligence. The AI does not submit the form.
Instead, the Medical Assistant reviews the clean, structured output, confirms its accuracy against the original chart, and then performs the final submission. This ensures that accountability remains human, while the “heavy lifting” of data mining is handled by code.
VII. Impact: Better Software as a Form of Care
The results in practice have been transformative:
- Time Savings: Reduced chart-review time by over 70%.
- Consistency: Every submission now uses the same high-standard evidence base.
- Reduced Burnout: Staff spend less time digging through notes and more time interacting with patients.
- Patient Outcomes: Faster authorizations mean faster treatment.
VIII. Final Reflection: Why Doctors Should Build
This project wasn’t the result of a multi-million dollar venture-backed startup. It was a physician seeing a systems problem and applying a software-thinking mindset to fix it.
Doctors don’t need to become full-time engineers. We need to become problem-literate.
Sometimes the fastest way to care for a high-risk patient isn’t a new drug or a more expensive ultrasound machine—it’s better software built by the people who actually do the work.
Chukwuma I. Onyeije, MD, FACOG Medical Director, Atlanta Perinatal Associates and Founder, CodeCraftMD