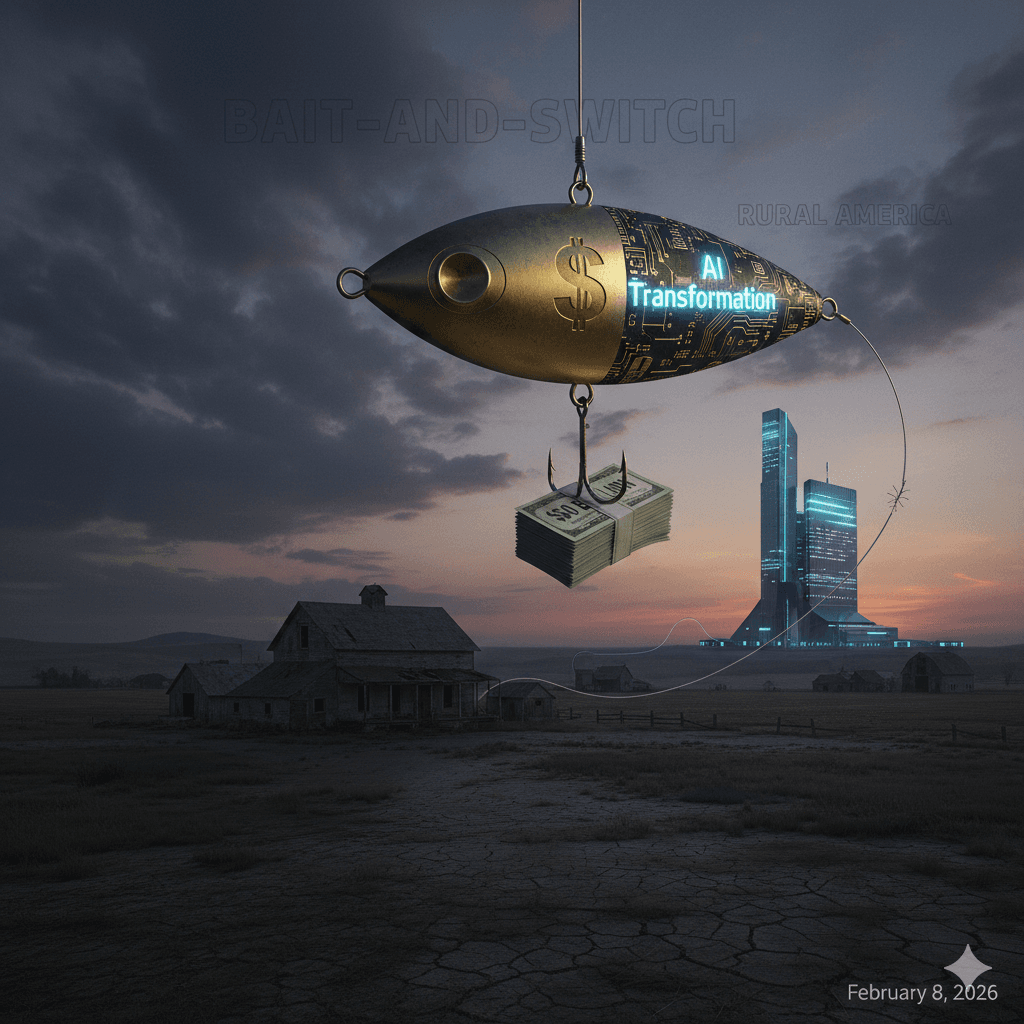
Part 1: The $50 Billion Bait-and-Switch
How AI “Transformation” Became Cover for Abandoning Rural America
By Chukwuma Onyeije, MD, FACOG
Maternal-Fetal Medicine Specialist & Founder, CodeCraftMD

The pitch sounds good if you don’t look too closely.
Fifty billion dollars for “AI transformation” in rural healthcare. Digital assistants bringing 24/7 medical expertise to communities that can’t retain physicians. The promise of technology bridging America’s healthcare deserts.
As a physician who codes, I should be celebrating. This is my domain—the intersection of clinical medicine and artificial intelligence. But instead, I’m watching the biggest policy con job of the decade unfold in real-time.
And the math tells you everything you need to know.
Follow the Money (Because They Hope You Won’t)
The Rural Healthcare Transformation Program (RHTP), buried in Public Law 119-21, allocates $50 billion over five years—roughly $10 billion annually through 2030—exclusively for AI implementation in rural settings.
Sounds transformative. Until you read the fine print.
That same legislation cuts $137 billion from rural Medicaid over the same period.
Let me spell that out for the folks in the back: For every dollar in “AI transformation,” rural communities lose $2.74 in actual healthcare coverage.
This isn’t innovation. It’s liquidation with a better marketing budget.
(Source: Trade-offs Health Policy Podcast, University of Pennsylvania Leonard Davis Institute analysis, January 2025)
The Technical Reality Vendors Won’t Tell You
I build AI tools. I understand their power and their profound limitations. So when I read that these $50B must fund “digital clinic assistants” and “AI avatars” as primary care interfaces, every alarm bell in my developer brain goes off.
Because here’s what an AI avatar fundamentally cannot do:
Perform physical diagnosis. No Large Language Model can palpate a gravid uterus to assess fundal height. No computer vision system can perform Leopold maneuvers to determine fetal position. No generative AI can auscultate heart sounds or check cervical dilation.
Execute interventions. An avatar can’t start an IV, can’t stabilize a patient in diabetic ketoacidosis, can’t perform an emergency cesarean section when a placental abruption presents at 2 AM.
Bridge the referral gap. This is the part that enrages me as a maternal-fetal medicine specialist. An AI can correctly identify a patient with preeclampsia with severe features. It can even generate the perfect evidence-based treatment protocol. But if the nearest hospital with Labor & Delivery capability just closed due to Medicaid funding cuts, the AI has simply provided a more efficient way to document preventable maternal mortality.
We’re not building tools to save rural healthcare. We’re building sophisticated triage systems for managed decline.
The Vendor Gold Rush (While Hospitals Bleed Out)
Here’s the truly perverse incentive structure:
The RHTP explicitly prohibits using these funds to:
- Cover hospital operational deficits
- Retain nursing staff
- Maintain obstetric units
- Subsidize physician recruitment
But it requires spending on:
- Enterprise AI licensing agreements
- “Avatar” interface systems
- Vendor implementation services
- Multi-year software contracts
You see the pattern, right? This isn’t a rural health investment. It’s a $50B subsidy for the enterprise AI industry, laundered through dying hospitals.
Rural administrators—already underwater from declining reimbursements—are being forced into a devil’s bargain: Fire your clinical staff to afford the AI systems that will replace them, or lose access to federal funding entirely.
A High-Risk OB Perspective on Low-Tech Realities
Let me give you a concrete scenario from my practice:
A 32-year-old G2P1 at 34 weeks presents with severe headache, right upper quadrant pain, and blood pressure 168/110. Her platelet count is 87,000.
An AI avatar can:
- Correctly diagnose HELLP syndrome
- Generate the appropriate workup
- Recommend magnesium sulfate and delivery planning
- Document everything in pristine SOAP format
An AI avatar cannot:
- Administer IV magnesium
- Perform the necessary cesarean delivery
- Manage postpartum hemorrhage
- Provide actual obstetric care
If her local hospital’s OB unit closed last year due to Medicaid cuts, that AI consultation is just expensive performance art. The patient still has to drive 90 miles in active HELLP syndrome to reach definitive care—if she makes it.
This is the “transformation” we’re funding. Not care. Choreographed abandonment.
The Physician-Developer’s Dilemma
For those of us in the MD-coder community, this presents an ethical crisis.
We entered this space to empower clinicians—to build tools that extend our capabilities, automate administrative waste, and let us focus on the human work only we can do.
But the RHTP is asking us to build something fundamentally different: replacement systems for when the human clinicians are gone.
We’re being asked to code the infrastructure for a future where rural Americans have access to simulated healthcare while urban and suburban communities get actual physicians.
I won’t do it. And I’m arguing you shouldn’t either.
What Actual Transformation Would Look Like
If this were genuinely about innovation rather than cost-shifting, the policy would look completely different:
Instead of: $50B in vendor contracts for AI avatars
Fund: Direct support for rural physician salaries with AI augmentation tools
Instead of: Prohibited use for hospital operations
Fund: Hybrid models where AI handles documentation/triage and humans handle clinical care
Instead of: Enterprise licensing mandates
Fund: Open-source clinical AI tools built BY rural physicians FOR rural contexts
The technology isn’t the problem. The deployment model is the scam.
The Bottom Line
As physician-developers, we have a choice to make.
We can build tools that support struggling rural providers—AI that handles prior authorizations, automates clinical documentation, flags high-risk patients for physician review, and genuinely extends clinical capacity.
Or we can build elaborate avatars that provide the appearance of care while actual healthcare infrastructure collapses.
One path uses technology to amplify human capability. The other uses technology to justify human abandonment.
I know which side I’m coding on.
Next in this series: “Building AI for Rural Reality” – How physician-developers can create tools that actually support rural providers instead of replacing them.
About the Author
Chukwuma Onyeije, MD, FACOG is a board-certified Maternal-Fetal Medicine specialist and Medical Director at Atlanta Perinatal Associates. He founded CodeCraftMD, an AI-powered medical documentation platform, and writes at lightslategray-turtle-256743.hostingersite.com about the intersection of clinical practice and software development. His work focuses on physician-built AI solutions that augment rather than replace clinical judgment.
Tags
#RuralHealthcare #AIinMedicine #HealthPolicy #MedicaidCuts #HealthEquity #PhysicianDevelopers #ClinicalAI #HealthcareInnovation #DigitalHealth #MaternalFetalMedicine #HighRiskOB #HealthIT #MedicalAI #RuralMedicine #HealthcareAccess
SEO Keywords
- Rural healthcare AI transformation
- Medicaid cuts rural hospitals
- AI avatars healthcare limitations
- Physician perspective AI implementation
- Rural hospital closures 2025
- Healthcare artificial intelligence policy
- Digital health equity
- Rural obstetric care access
- AI vs human healthcare
- Physician-built AI tools
- Rural Healthcare Transformation Program
- Healthcare AI vendor contracts
Meta Description (155 characters):
“A maternal-fetal medicine specialist exposes the $50B rural AI program that cuts $137B in Medicaid—and why physician-developers must push back.”
Title Tag (60 characters):
“The $50B AI Bait-and-Switch Destroying Rural Healthcare”